Page Links:
A. Optical terms and concepts:
Here are some of these terms:
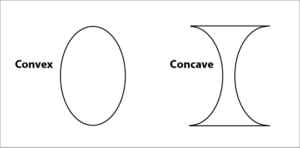
A: Reflection <-> Refraction
B: Convex <> Concave
C: focal line, focal point, focal lengthSclera:
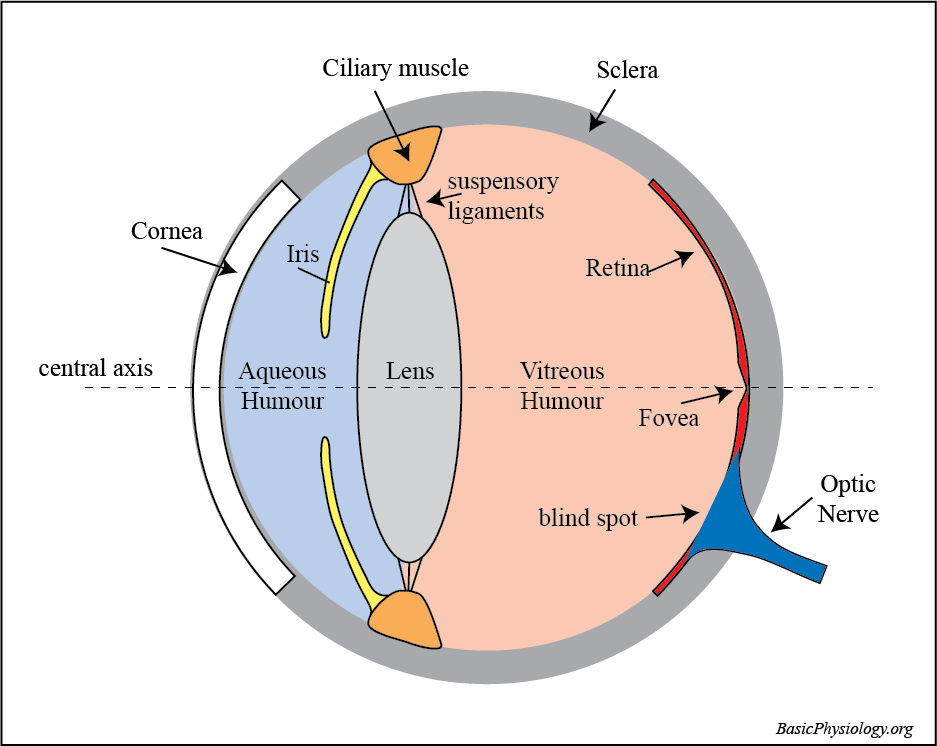
the outer ‘skeleton’ of the eye.
Lens:
provides for a variable refraction.
Aqueous Humour:
fluid in front of the lens that provides for the intra-ocular pressure.
Retina:
contains the photoreceptors that are sensitive to the light and the nerve cells that communicate to the optic nerve and the brain.
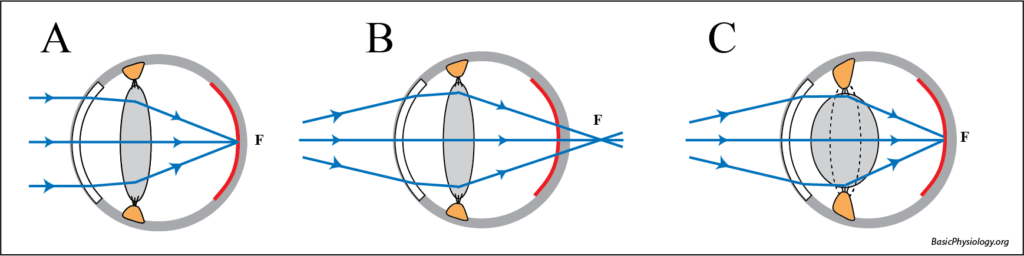
Accommodation occurs when the eye changes the shape (curvature) of the eye to focus on objects close to or distant from the eye
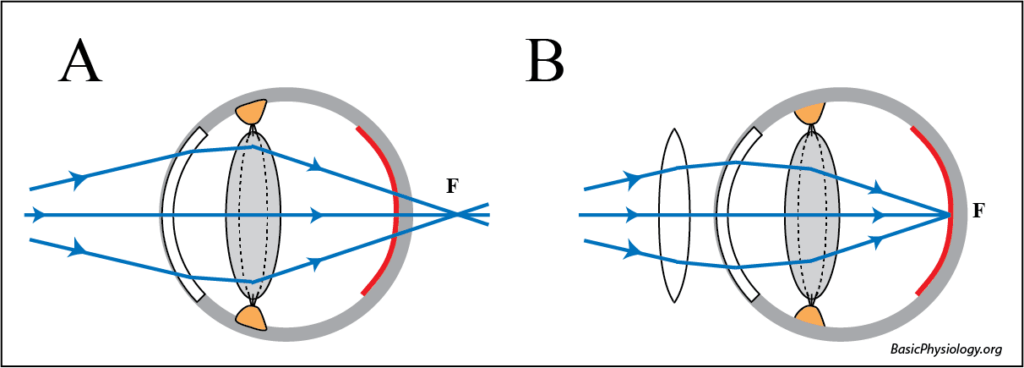
Fig A. The eye is not accommodated.
In this situation, when the light travels in parallel rays, from far away, then the focus will fall on the fovea.
Fig B. When the light rays diverge
because the image is close to the eye (for example when one is reading), then, if nothing changes, the focus will fall behind the fovea, and the picture will be unclear.
Fig C. Accommodation.
To move the focus towards the fovea, the curvature of the lens must become more convex. This will increase the refraction of the lens and the light rays will converge on the fovea.
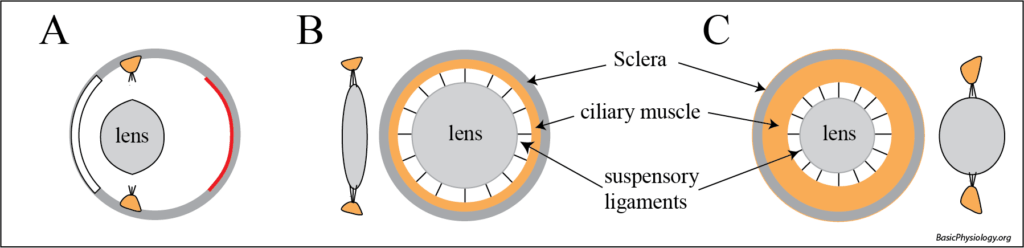
Fig A. The natural recoil of the lens.
The lens, by itself, when cut of from the suspensory ligaments, is very convex (close to a sphere). It is, in the eye, stretched by the suspensory ligaments and the ciliary muscle into a thinner and lesser convex lens.
Fig B. Non-accommodated.
In this situation, the ciliary muscle is resting and stretches the ligaments, thereby also stretching the lens into a less-convex shape. This is the situation when looking far away.
Fig C. Accommodation.
When the lens has to accommodate (=reading), then the ciliary muscle contracts, the ‘hole’ in the muscle becomes smaller, the suspensory ligaments move towards the centre, and this allows the lens to become more convex.
Presbyopia.
In some eyes, especially in older people, the elasticity of the eye has decreased and the lens is no longer as convex as before.
Fig A. Maximum accommodation.
In that situation, a maximum accommodation (= contraction of the ciliary muscle) will still not be able to move the focus to the fovea and the image remains blurry. This situation is called presbyopia.
Fig B. Reading lenses.
This situation can be helped by using reading lenses, which are convex lenses (positive “+” lenses). They help in breaking more the diverging light rays to focus the light rays on the fovea.
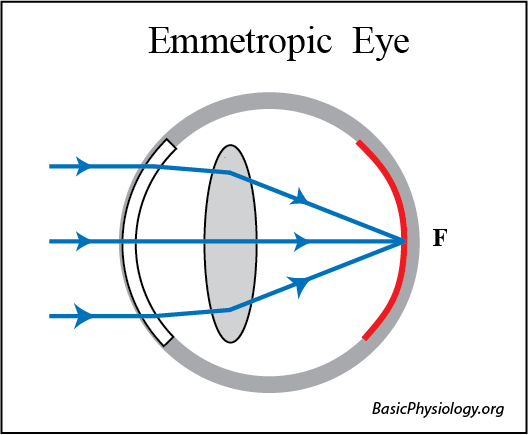
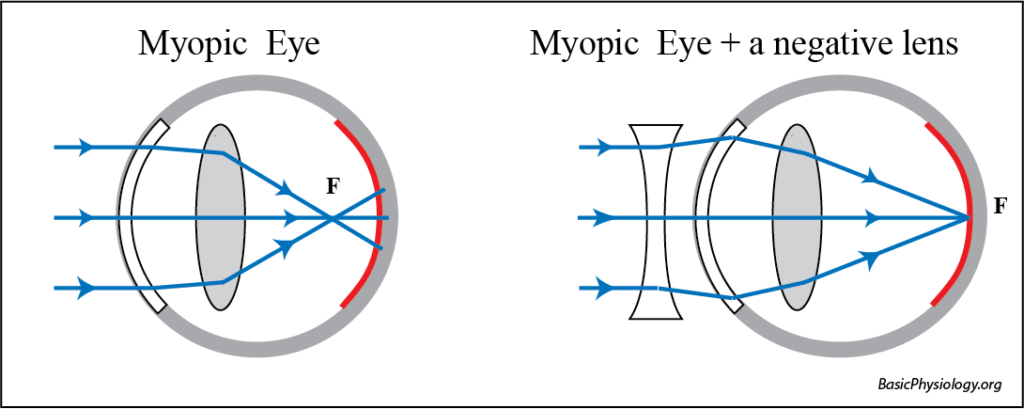
In an emmetropic eye, light rays from far away (thereby creating parallel light rays) fall on the fovea. These patients do not need glasses to look far away.
Note that such a person can look sharp at images close to the eye (like reading) as this will move the focus towards the fovea. That is why these people are called “near-sighted”
In a hyperopic eye (=hyperopia), parallel light rays will fall “behind” the retina. To help these patients, a convex (“+”) lens is required which will help ‘break’ the light rays more.
Note that these patients can (and do) help themselves by accommodating their lens. This will also move the focus onto the fovea. They do this automatically and therefore often they don’t know that they have a refraction anomaly. They are therefore called “farsighted”. They will often complain of headaches or tiredness as their ciliary muscle contracts all the time.
1.
In the previous refraction anomalies (myopia and hyperopia) the curvature or the bending of the lens was the same at all angles. In some patients however, the degree of curvature is different between two (or more) different angles. In the diagram, this is illustrated by a flat convex lens that is more curved from top to bottom then from left to right. An exaggerated example of such a curvature is the surface of an egg; more curved in one direction then in another.
2.
The consequence of astigmatism is that there is not one focal point but several, located between one extreme and the other. Such patients require specially designed lenses in which the curvature of the lens is adapted to their astigmatism. This can be seen in some lens prescription as follows: +1.5 D at 100 degrees and +0.5 D at 45 degrees.
Cataract:
In some patients, the lens becomes, gradually, less-transparent. There are many reasons for this to happen including metabolic diseases, congenital or old age. Because the lens becomes gradually less transparent, the patients will see the images more and more blurred. The therapy is to remove the lens and to replace it with a new artificial intra-ocular lens.
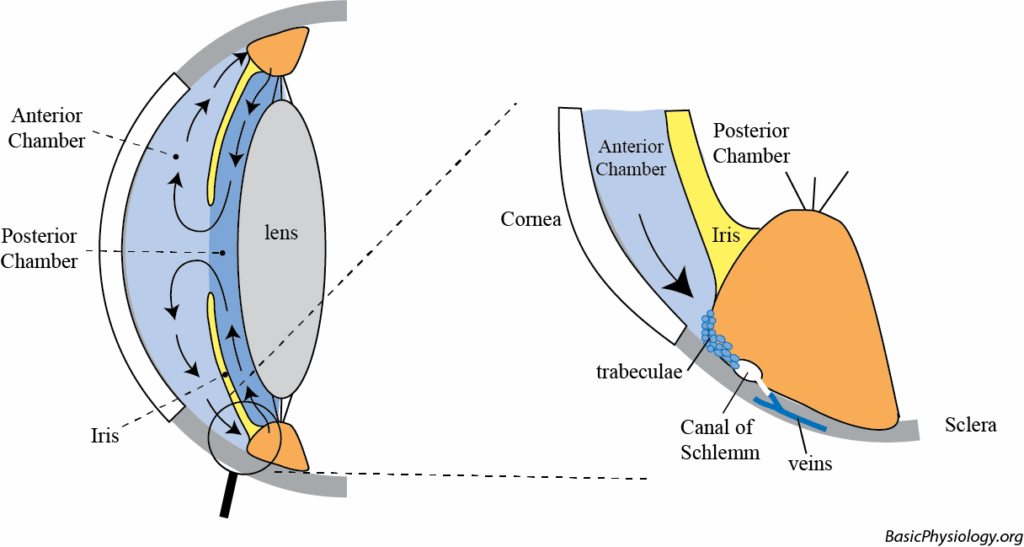
Anterior and Posterior Chamber:
The space between the cornea and the lens is filled with a fluid (= the aqueous humour). The iris divides this fluid in two spaces; a posterior and an anterior chamber (chamber = room).
Intra-ocular circulation 1:
The ocular fluid is secreted by the ciliary body into the posterior chamber. From there, it flows through the pupil (= the opening between the iris), into the anterior chamber. There, it flows back into the corner between the sclera, the base of the iris and the ciliary body.
Intra-ocular circulation 2:
In this (narrow) angle there are trabeculae that filter the fluid into a canal (= canal of Schlemm) which, in turn, drains into a local vein.
Intra-ocular circulation 3:
In this manner, fresh fluid (with nutrients etc) is constantly flowing through the anterior part of the eye and, by diffusion, through the lens and the vitreous body towards the retina.
Intra-ocular pressure:
This also provides for a small pressure in the eye of about 5-10 mmHg. This keeps the eye in the shape of a ball and all its internal structures (lens etc) in place. If the pressure were too low, then the eyeball would collapse and vision becomes blurred.
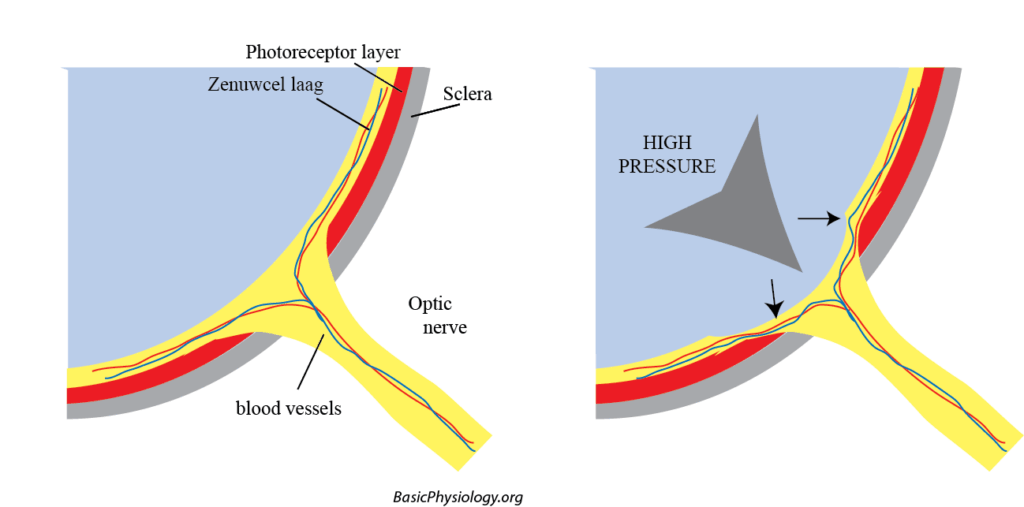
Glaucoma 1:
If the pressure gets too high (=glaucoma), then another danger arises. A too high pressure (> 20 mmHg) will impede or block blood flow through the optic nerve. These vessels are crucial as they perfuse the retina.
Glaucoma 2:
If the perfusion is stopped, the photoreceptor cells will become ischemic (= no blood) and die. The person will become blind.
Glaucoma 3:
An acute glaucoma (pressures 70-80 mmHg) can occur if there is an obstruction of the flow to the canal of Schlemm. A chronic glaucoma (pressures 20-30 mmHg) occurs when the obstruction is limited.